Prostate cancer is a common form of cancer that affects men. It is typically slow-growing and often does not cause any symptoms in its early stages, which is why routine screening is important for early detection and treatment.
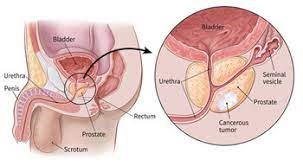
The prostate is a small gland located below the bladder and in front of the rectum. It produces fluid that makes up part of semen. Prostate cancer occurs when abnormal cells grow uncontrollably in the
prostate gland.
How common is Prostate Cancer?
Prostate cancer is the most common cancer in men in the UK, with around 50,000 new cases diagnosed each year.
The incidence of prostate cancer in the UK has been steadily increasing over the past few decades. In the 1970s, around 4,000 men were diagnosed with the disease each year. By the 1990s, this had risen to around 20,000 men per year, and by the early 2000s, the number had increased to over 35,000 men per year.
Currently, around one in eight men in the UK will be diagnosed with prostate cancer at some point in their lifetime. The disease is more common in older men, with the majority of cases occurring in men over the age of 50. In fact, around 6 in 10 cases of prostate cancer in the UK are diagnosed in men over the age of 65. However, it is important to note that prostate cancer can also affect younger men, even though this is less common.
It is important to note that while the incidence of prostate cancer in the UK has been increasing, the mortality rate from the disease has been decreasing. This is largely due to improvements in screening, diagnosis, and treatment, which have enabled more cases to be detected at an early stage, when they are more treatable.
What causes Prostate Cancer?
There are several risk factors that may increase a man’s risk of developing prostate cancer. These include:
- Age: As mentioned, prostate cancer is more common in older men. Age is one of the most significant risk factors for prostate cancer. The disease is very rare in men under the age of 50, but the risk increases significantly as men get older. In fact, around 70% of all cases of prostate cancer are diagnosed in men over the age of 65.
- Family history: Family history is another important risk factor for prostate cancer. Men who have a close relative, such as a father or brother, who has been diagnosed with the disease are at a higher risk of developing it themselves. This risk is further increased if the relative was diagnosed at a young age or if multiple family members have been affected.
- Ethnicity: Ethnicity also plays a role in prostate cancer risk. Black men are at a higher risk of developing the disease than men of other ethnicities, with around one in four black men being diagnosed with prostate cancer at some point in their lifetime. The reasons for this increased risk are not fully understood, but it may be due to differences in genetic and/or environmental factors.
- Lifestyle: Finally, lifestyle factors such as diet and exercise can also influence the risk of prostate cancer. Men who consume a diet high in red meat and saturated fat are thought to be at a higher risk of developing the disease, while those who eat a diet rich in fruits and vegetables may have a lower risk. Regular exercise has also been shown to reduce the risk of prostate cancer.
What are the signs and symptoms of Prostate Cancer?
In its early stages, prostate cancer may not cause any symptoms, which is why it’s important for men to get regular prostate cancer screenings. However, as the cancer grows, it can cause a variety of symptoms, including:
- Difficulty urinating: One of the most common symptoms of prostate cancer is difficulty urinating. This can include a weak or interrupted urine flow, straining to urinate, and feeling like you need to urinate more often than usual, especially at night.
- Blood in urine or semen: Another symptom of prostate cancer is the presence of blood in urine or semen. This can be a sign that the cancer has spread to other parts of the body, such as the bladder or the seminal vesicles.
- Painful ejaculation: Men with prostate cancer may experience pain or discomfort during ejaculation, which is caused by the cancer pressing on the nerves that control ejaculation.
- Erectile dysfunction: Prostate cancer can also cause erectile dysfunction, or the inability to achieve or maintain an erection. This is because the cancer can damage the nerves and blood vessels that are necessary for an erection.
- Back, hip, or pelvic pain: As prostate cancer progresses, it can spread to other parts of the body, including the bones. This can cause pain in the back, hips, or pelvis.
If you experience any of these symptoms, it is important to see your GP right away. While these symptoms may be caused by conditions other than prostate cancer, it is always best to get them checked out..
How is Prostate Cancer diagnosed?
There are several tests and investigations that may be used to diagnose and stage prostate cancer. These include:
- Digital rectal exam (DRE): This is a physical exam in which a healthcare provider uses a lubricated, gloved finger to feel the prostate gland through the rectum. Abnormalities in the size, shape, or texture of the prostate gland may indicate the presence of cancer.
- Prostate-specific antigen (PSA) test: This is a blood test that measures the level of PSA, a protein produced by the prostate gland. High levels of PSA may indicate the presence of prostate cancer or other conditions, such as an enlarged prostate or inflammation.
- Imaging tests: Imaging tests, such as a multi-parametric magnetic resonance imaging (MRI) or a computed tomography (CT) scan, may be used to help determine the extent and stage of the cancer. These tests can also help guide treatment decisions.
- Prostate Biopsy: If a DRE or PSA test suggests the presence of prostate cancer, a biopsy may be performed to confirm the diagnosis. During a biopsy, a small sample of prostate tissue is removed and examined under a microscope for signs of cancer.
- Bone scan: A bone scan may be used to determine if the cancer has spread to the bones. During a bone scan, a small amount of radioactive material is injected into the bloodstream, which is then detected by a special camera.
- PMSA PET scan: Early detection and accurate staging are critical to effective treatment, which is why advanced imaging techniques such as positron emission tomography (PET) scanning are increasingly being used. One type of PET scan that is commonly used in the diagnosis and staging of prostate cancer is the prostate-specific membrane antigen (PSMA) PET scan. This test uses a radioactive tracer that binds to the PSMA protein, which is found at high levels on the surface of prostate cancer cells. During a PSMA PET scan, the tracer is injected into the bloodstream and then detected by a special camera that creates detailed images of the prostate gland and surrounding tissues. This can help identify the location and extent of cancerous tissue, as well as any areas where the cancer may have spread.PSMA PET scans are particularly useful in detecting small amounts of cancerous tissue, as well as identifying cancer that may have spread to lymph nodes or other parts of the body. This information can help guide treatment decisions and improve outcomes.
What are the stages of Prostate Cancer?
In the UK, prostate cancer is typically staged using the TNM system, which stands for Tumour, Node, Metastasis.
Here are the stages of prostate cancer:
Stage I: At this stage, the cancer is only found in the prostate gland and is considered small and localized. There are no signs or symptoms of the cancer, and it’s typically detected through a routine prostate-specific antigen (PSA) test or digital rectal exam (DRE).
Stage II: At this stage, the cancer is still contained within the prostate gland but is larger and more advanced than in Stage I. There may still be no signs or symptoms of the cancer, or there may be mild symptoms such as difficulty urinating.
Stage III: At this stage, the cancer has started to spread beyond the prostate gland and may have invaded nearby tissues or organs. There may be more noticeable symptoms at this stage, such as frequent urination or blood in the urine.
Stage IV: At this stage, the cancer has spread to other parts of the body, such as the bones or lymph nodes. Symptoms may include bone pain, weight loss, and fatigue.
It’s important to note that not all cases of prostate cancer progress through all of these stages. Some men may be diagnosed with Stage IV prostate cancer right away, while others may never progress beyond Stage I or II.
How is Prostate Cancer treated?
Treatment for prostate cancer depends on the stage and severity of the cancer. Options may include watchful waiting, surgery to remove the prostate gland, radiation therapy, and hormone therapy. Your urologist can recommend the best treatment plan for you based on your individual needs.
- Active surveillance: This approach involves monitoring the cancer with regular PSA tests and biopsies but not immediately treating it. This option is typically recommended for men with early-stage prostate cancer who have a low risk of the cancer spreading.
- Surgery: Surgery to remove the prostate gland is another treatment option for prostate cancer. The most common type of surgery is called radical prostatectomy, which can be done through open surgery or minimally invasive laparoscopic surgery. This procedure is typically recommended for men with early-stage prostate cancer.
- Radiation therapy: Radiation therapy uses high-energy beams to kill cancer cells. It can be delivered externally through a machine or internally through radioactive seeds placed directly in the prostate gland. Radiation therapy is typically recommended for men with early-stage or locally advanced prostate cancer.
- Hormone therapy: Hormone therapy works by reducing the levels of testosterone in the body, which can slow the growth of prostate cancer. This treatment is typically recommended for men with advanced prostate cancer or for those who are not candidates for surgery or radiation therapy.
- Chemotherapy: Chemotherapy involves the use of drugs to kill cancer cells. This treatment is typically recommended for men with advanced prostate cancer that has spread to other parts of the body.
- Immunotherapy: Immunotherapy is a type of treatment that works by boosting the immune system to help fight cancer cells. This treatment is still being studied for prostate cancer and is typically reserved for men who have not responded to other treatments.
It’s important to note that each treatment option has its own risks and benefits, and the decision on which treatment to use should be made in consultation with a multidisciplinary team (MDT). Additionally, some men may require a combination of treatments to effectively manage their prostate cancer.
What is the life expectancy of a man with Prostate Cancer?
The outlook for men with prostate cancer varies depending on many factors, such as the stage and grade of the cancer, the age of the patient, and their overall health.
It’s important to note that prostate cancer is often a slow-growing cancer and may not cause symptoms for many years. Many men diagnosed with early-stage prostate cancer are able to live for many years without their cancer causing any significant health problems. However, in some cases, prostate cancer can be more aggressive and may spread to other parts of the body.
According to the latest statistics from Cancer Research UK, the 10-year survival rate for men with prostate cancer in the UK is around 84%. This means that 84% of men diagnosed with prostate cancer are still alive 10 years after their diagnosis. However, it’s important to note that this figure is an average and does not take into account individual factors that may affect life expectancy.
For example, men with early-stage prostate cancer may have a higher survival rate than men with advanced-stage prostate cancer. Additionally, older men and men with other health conditions may have a shorter life expectancy than younger, healthier men with prostate cancer.
Conclusion:
Prostate cancer is a significant health concern in the UK, particularly for men over the age of 50. By understanding the risk factors and symptoms of prostate cancer, you can take steps to reduce your risk and seek prompt medical attention if you suspect you may have the disease. If you are over 50 and have any of the risk factors mentioned above, it is recommended that you speak to your GP about prostate cancer screening.
Author: Mr Neil A Haldar MBBS MD FRCS
Consultant Urological Surgeon
The Pelvic Specialists
